Several groups have reported qualitative associations between obstructive sleep apnea (OSA) and coronary plaque1-3; however, a recent study published in Chest4 provides a compelling set of quantitative data showing the OSA was independently associated with coronary plaque burden, specifically of the type that is most associated with coronary events.
Plaque volume and composition predict acute coronary syndrome
To understand the significance of the Chest paper, we must first briefly review the application of coronary computed tomography (CT) angiography in assessing coronary plaques. Coronary CT angiography is a noninvasive procedure that provides an accurate and detailed estimate not only of plaque burden, but also of plaque composition. Previous studies have shown that plaque burden, that is coronary plaque volume, predicts the risk of future acute coronary events.5,6
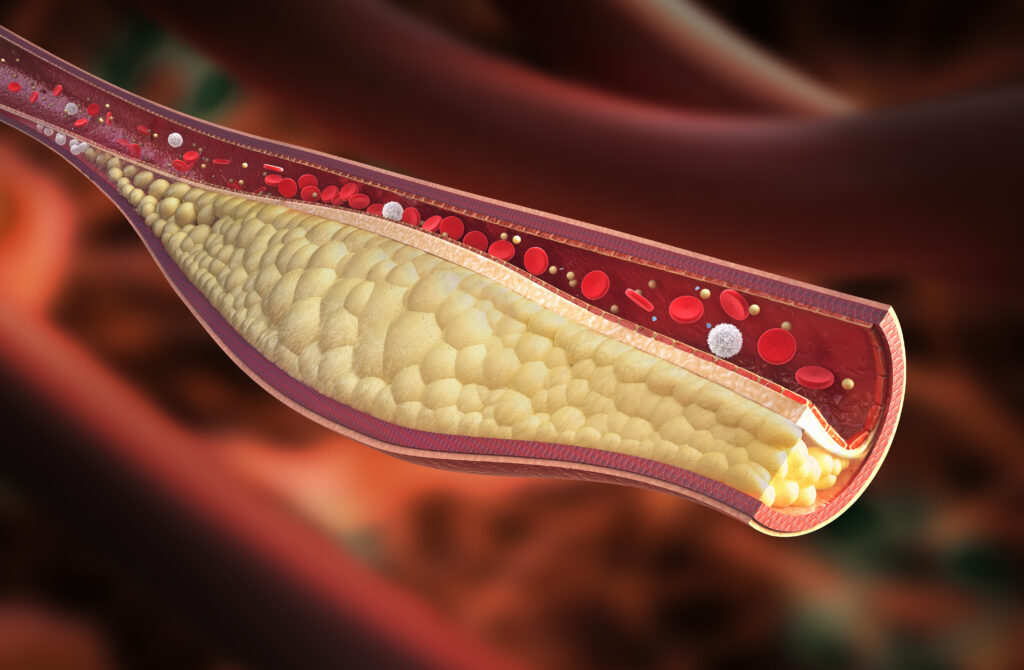
This is an intuitive and important association, but it is slightly less interesting than the information that can be gleaned from coronary CT angiography on coronary plaque composition. Plaque rupture, which is the event that is believed to immediately precede an acute coronary event, takes place most often in plaques that have a large, lipid-rich, necrotic core covered by a thin fibrous cap.7,8 These inflamed structures can be viewed on a coronary CT angiogram as low-density noncalcified plaques.9 Thus, coronary plaque volume, especially the presence of low-density noncalcified plaques, predicts the risk of plaque rupture and acute coronary syndrome.
Study design
The researchers examined data from 692 patients who had both sleep apnea testing and coronary CT angiography results available. Coronary CT angiography was performed according to standard procedures using iopromide contrast (Ultravist®). Associations between obstructive sleep apnea severity and the presence, volume, and composition of plaque were examined with multivariable logistic and linear regression analyses. Obstructive sleep apnea severity was defined by the apnea-hypopnea index, or AHI, which was the mean number of apnea and hypopnea events per hour of sleep. As is standard, an AHI between 5 and 15 events per hour was defined as mild obstructive sleep apnea; moderate obstructive sleep apnea was defined as between 15 and 30 events per hour; and severe obstructive sleep apnea was defined as more than 30 events per hour. The researchers also tracked the Epworth Sleepiness Scale to assess daytime sleepiness.
Obstructive sleep apnea is a severity-dependent risk factor for coronary plaques
Patients with moderate or severe obstructive sleep apnea, that is more than 15 apnea and hypopnea events per hour of sleep, were significantly more likely to have coronary plaques than those with no or only mild obstructive sleep apnea (P=0.037).4 Moreover, patients with moderate or severe AHI scores were more likely than people with less severe disease to have noncalcified plaque (P=0.032) and specifically low-density noncalcified plaque, (P=0.030), which is the highly unstable form of coronary plaque.
When analyzed as a continuous variable, the severity of obstructive sleep apnea (AHI) correlated with plaque volume, including low-density noncalcified plaque. Indeed, an oxygen desaturation index of 3% (P=0.005) and percentage of time during sleep in which oxygen saturation was less than 90% (P=0.017) also positively predicted low-density noncalcified plaque.
Interestingly, mean scores among people with no or mild OSA were only 1 point lower than those with moderate or severe disease, suggesting that daytime sleepiness is not a robust screen for potential sleep disordered breathing.
Considerations and limitations
This study provides even more support for the association between moderate and severe obstructive sleep apnea and the risk of acute coronary syndrome. Some considerations should be mentioned. First, this cross-sectional study design shows an association, but cannot indicate causality. Second, each of these patients had both a sleep apnea study and coronary CT angiography, so the results may not be generalizable. Nevertheless, the number of studies showing a strong, positive association between sleep apnea severity and cardiovascular risk is impressive. Moreover, a plausible mechanism exists: sympathetic activation, oxidative stress, and sleep fragmentation are known to be damaging to the endothelium and lead to the formation of atherosclerotic plaques.10,11
Implications for cardiology practice
Despite the fact that all patients in the study underwent coronary CT angiography, most did not have known coronary artery disease, and they were relatively young (mean age of 55).4 The authors suggest this indicates early-stage atherosclerosis. Given that daytime sleepiness is a rather poor screening tool for obstructive sleep apnea and the apnea-hypopnea index of sleep apnea strongly correlates with rupture-prone, low-density noncalcified plaques, cardiologists should strongly consider incorporating sleep apnea testing in all patients at risk for coronary artery disease. It has not yet been shown that positive airway treatment can halt or reverse advancing coronary artery disease, but accurate at-home sleep apnea testing has made sleep apnea testing and diagnosis nearly effortless for cardiologists and patients alike. Ordering an inexpensive, simple, and convenient test to identify a potential contributor to or cause of acute coronary syndrome seems like a straightforward choice.
References
3. Turmel J, Sériès F, Boulet L-P, et al. Relationship between atherosclerosis and the sleep apnea syndrome: an intravascular ultrasound study. Int J Cardiol. 2009;132(2):203-209. doi: 10.1016/j.ijcard.2007.11.063
4. Lu M, Fang F, Wang Z, et al. Association between OSA and quantitative atherosclerotic plaque burden: a coronary CT angiography study. Chest. 2021;160(5):1864-1874. doi: 10.1016/j.chest.2021.07.040
5. Williams MC, Kwiecinski J, Doris M, et al. Low-attenuation noncalcified plaque on coronary computed tomography angiography predicts myocardial infarction: results from the multicenter SCOT-HEART trial (Scottish Computed Tomography of the HEART). Circulation. 2020;141(18):1452-1462. doi: 10.1161/CIRCULATIONAHA.119.044720
6. Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54(1):49-57. doi: 10.1016/j.jacc.2009.02.068
7. Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation. 2003;108(14):1664-1672. doi: 10.1161/01.CIR.0000087480.94275.97
8. Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation. 2003;108(15):1772-1778. doi: 10.1161/01.CIR.0000087481.55887.C9
9. Voros S, Rinehart S, Qian Z, et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging. 2011;4(5):537-548. doi: 10.1016/j.jcmg.2011.03.006
10. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College Of Cardiology Foundation scientific statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118(10):1080-1111. doi: 10.1161/CIRCULATIONAHA.107.189375
11. Kohler M, Stradling JR. Mechanisms of vascular damage in obstructive sleep apnea. Nat Rev Cardiol. 2010;7(12):677-685. doi: 10.1038/nrcardio.2010.145
10. Tanaka N, Tanaka K, Hirao Y, et al. Home Sleep Apnea Test to Screen Patients With Atrial Fibrillation for Sleep Apnea Prior to Catheter Ablation. Circ J. 2021;85(3):252-260. 10.1253/circj.CJ-20-0782
11. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52(8):686-717. 10.1016/j.jacc.2008.05.002
12. Zancanella E, do Prado LF, de Carvalho LB, Machado Junior AJ, Crespo AN, do Prado GF. Home sleep apnea testing: an accuracy study. Sleep Breath. 2021. 10.1007/s11325-021-02372-6
13. Defaye P, de la Cruz I, Marti-Almor J, et al. A pacemaker transthoracic impedance sensor with an advanced algorithm to identify severe sleep apnea: the DREAM European study. Heart Rhythm. 2014;11(5):842-848. 10.1016/j.hrthm.2014.02.011
14. Epstein M, Musa T, Chiu S, et al. Use of the WatchPAT to detect occult residual sleep-disordered breathing in patients on CPAP for obstructive sleep apnea. J Clin Sleep Med. 2020;16(7):1073-1080. 10.5664/jcsm.8406
15. Pillar G, Berall M, Berry R, et al. Detecting central sleep apnea in adult patients using WatchPAT-a multicenter validation study. Sleep Breath. 2020;24(1):387-398. 10.1007/s11325-019-01904-5
16. Mehra R, Wazni O. POINT: Should All Patients With Atrial Fibrillation Who Are About to Undergo Pulmonary Vein Ablation Be Evaluated for OSA? Yes. Chest. 2018;154(5):1008-1010. 10.1016/j.chest.2018.06.042
17. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071-2104. 10.1161/CIR.0000000000000040
