By Melih Alvo
Afib effects 6M lives1 in US and each year ~350.000 patients undergo ablation procedure to treat this condition. Intracardiac AFib ablation is an invasive cardiac procedure, carrying some significant risk for complications, in particular these associated with the transeptal puncture and esophageal fistulas and it is associated with significant cost to the healthcare system and the patient. Unfortunately about 50% of AFIB patient that undergo their first ablation procedure experience reoccurrence of Afib2 within one year. There are multiple thoughts on the underlaying reasons for this big variability in outcome with much dialog and efforts focusing on the procedure itself. Recently, new data published have suggested one of the gaps may not be in the ablation lines but with another condition -sleep apnea and the implications of it on the heart tissue and physiology.
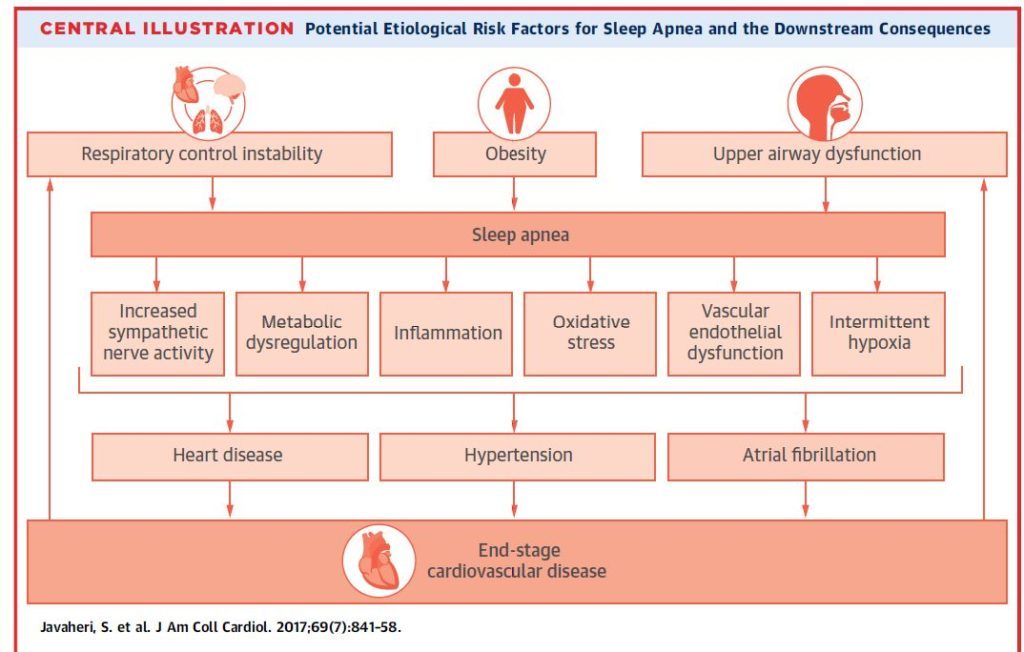
Recently accelerated number of new clinical studies shows the effect of sleep apnea on Afib recurrence. On March 2017 the American College of Cardiology invited a review paper discussing the evidence demonstrating the causality relationships of sleep apnea driving higher AFIB burden. The below illustration is a recreation of similar diagram featured in this publication:
In light of all these information’s, Dr. Elad Anter from Boston Beth Israel Deaconess Medical Center, a Harvard Medical Institute, recentlypublished yet another clinical study which may change the EPs approach to
Afib ablation.
In this multi-center prospective randomized study 86 patients with Paroxysmal Atrial Fibrillation defined under two groups; group one of 43 patients with diagnosed OSA and group two, 43 patients without OSA. Diagnosis was done both with traditional means and with the novel WatchPAT home sleep test technology. All patients undergo comprehensive mapping of their atrial substrate, PV trigger identification and PV Isolation and non-PV trigger mapping and ablation. In addition there were retrospective 2 control groups one without OSA and one with moderate OSA. Both of those groups underwent PVI alone without mapping and ablation of Non-PV triggers.
Findings of the study were amazing. After PV isolation, patients with OSA had significant increased incidence of clinically relevant additional Non PV triggers (4.8% vs. 11.6%; P=0.003) and patients with OSA who only underwent PV isolation without ablating non-PV triggers had increased risk of arrhythmia recurrence (83.7% vs. 64.0%; P=0.003). Also 1 year arrhythmia-free survival was similar between patients with and without OSA that undergo both PVI and non-PV triggers ablation (83.7% vs 81.4%; P=0.59)4
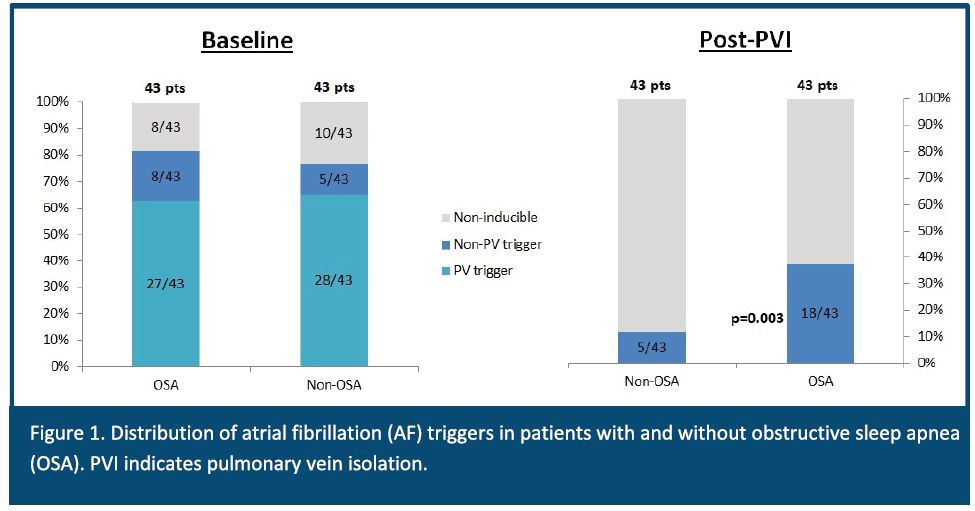
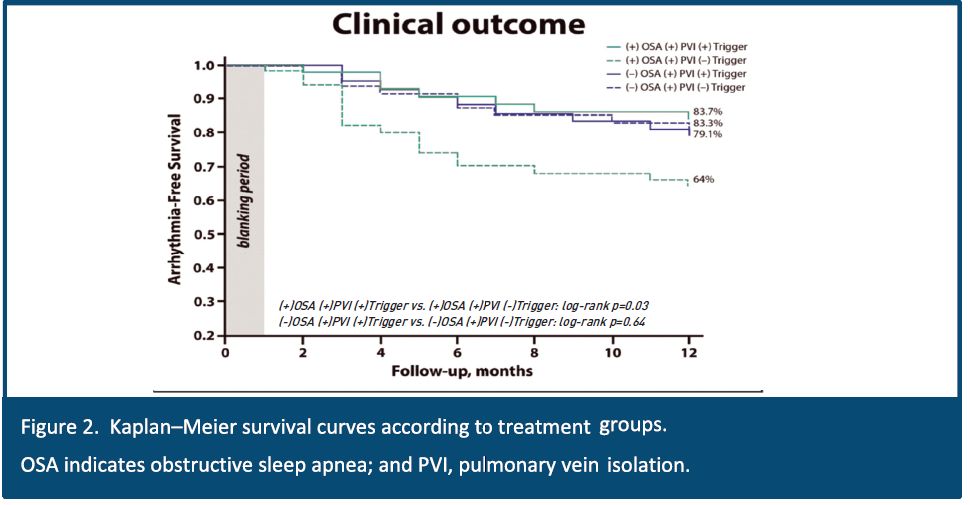
As conclusion, OSA is associated with structural and functional remodeling and increased incidence of non-PV triggers. Eliminating these triggers will improve arrhythmia free survival. In other words, patients with OSA have higher chance to have non-PV triggers4 and therefore require different approach to AF ablation. Knowing the patients OSA status prior to the ablation process become critical piece of information that may help to define the right ablation strategy.
In below link you may see the full article.
https://www.itamar-medical.com/wp-content/uploads/2019/12/e005407.full_.pdf
The WatchPAT Home Sleep Apnea monitor is an easy to use, effective and accurate tool for OSA diagnosis in AFib patients. Contact Us for more information about WatchPAT and our comprehensive “Total Sleep Solution” for Cardiology practices. www.cardiosleepsolutions.com
1 – Source: Seet & Chung, Anestsiology Clin 2010
2 – Effect of Obstructive Sleep Apnea Treatment on Atrial Fibrillation Recurrence
3 – Atrial substrate and triggers of paroxysmal Atrial Fibrillation in patients with obstructive sleep apnea
