In 2018, nearly half a million deaths in the United States included hypertension as a primary or contributing cause.1 Its prevalence is undeniable as nearly one out of two adults in the country suffer from this condition.2 We know that hypertension can contribute to many health ailments, such as heart disease and stroke, which is why we focus on the many factors that can lead to its development. However, when it comes to hypertension, one such factor often overlooked is abnormal sleep. This week is the National Sleep Foundation’s National Sleep Awareness Week, and since many individuals suffer from sleep disorders, it is important to know the association between sleep disorders and hypertension.
Sleep Disorders and Hypertension
The American Academy of Sleep Medicine and the Sleep Research Society recommend that adults sleep at least seven hours each night for well-being.3 As reported by the Centers for Disease Control and Prevention, one out of three American adults do not meet this criteria.4 One primary reason is the prevalence of sleep disorders in American society. The Cleveland Clinic states that about 70 million people in the United States suffer from sleep disorders.5
With many Americans not getting adequate sleep, the health repercussions that can follow are important to decipher. Seeing that high blood pressure is one of the most common conditions in the United States, compelling evidence links hypertension and sleep. According to a study by Daniel J. Gottlieb that involved 5,910 participants, it was found that the prevalence of hypertension was increased for participants who had less than the median mean of seven to eight hours of sleep per night, with a pronounced increase in prevalence seen in individuals who slept six hours or less per night.6 In fact, in a Mayo research study involving healthy adults, nightly sleep was restricted to four hours for nine nights and nine hours for nine nights—it was found that during the nine nights of four hours of sleep, participants had an average systolic blood pressure reading that was 10 millimeters of mercury (mm Hg) higher than the nine-hour sleep phase.7
For many people, a lack of adequate sleep is caused by sleep disruption from obstructive sleep apnea—a condition where there is a blockage of the upper airway that can lead to cessations of breathing during sleep. Patients who suffer from obstructive sleep apnea have elevated blood pressure during the night and are more likely to suffer from hypertension.
But how can an apnea disorder like obstructive sleep apnea induce hypertension? What is the etiology behind it? We are continuing to understand the intricacies of this relationship, but there are certain elements that we know to be relevant. During normal sleep, our blood pressure typically decreases by 10% to 20% than that of our daytime blood pressure.8 This decrease is often referred to as nocturnal dipping. Since sleep apnea can cause disturbances in this natural dipping phenomenon, blood pressure can stay higher for longer periods of time. It is also thought that since sleep helps regulate stress hormones, a lack thereof could lead to high blood pressure due to inadequate regulation.7
Why Sleep Should Be Discussed With Patients
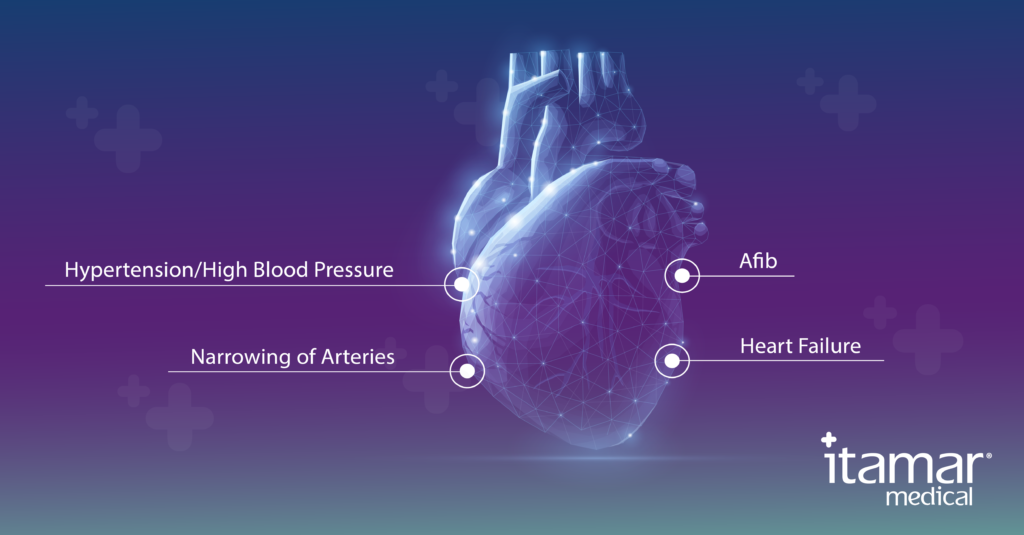
As a cardiologist, you are aware of the implications that hypertension can have on the heart. With millions of people suffering from sleep disorders, such as sleep apnea, it is possible that many patients who have hypertension may be suffering from sleep apnea or a lack of adequate sleep in general. The association between improper sleep and hypertension is important; therefore, sleep health must become a priority. Sleep apnea screening benefits your patients as sleep apnea is a relevant cardiac co-morbidity. However, discussing and screening for sleep apnea with your patients is not only important for hypertension but also for other conditions that can affect the heart. For example, atrial fibrillation is the most common arrhythmia diagnosed in clinical practice, and sleep disorders—especially sleep apnea – have been discovered to be a significant risk factor. Learn more about that specific link in our upcoming article on the relationship between sleep apnea and atrial fibrillation as we take a deeper dive into this relation.
Also, if you are looking for a remote sleep apnea management solution for your practice, check out our WatchPAT® TurnKey Program, where we provide a seamless pathway to ensure cardiovascular patients with sleep apnea are diagnosed effectively and can be treated in less than 2 weeks on average.
References:
- Facts About Hypertension. Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm. Published September 8, 2020. Accessed March 1, 2021.
- Estimated Hypertension Prevalence, Treatment, and Control Among U.S. Adults. Million Hearts. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Published February 5, 2020. Accessed March 1, 2021.
- Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. SLEEP. 2015;38(6):843-844. doi:10.5665/sleep.4716
- 1 in 3 adults don’t get enough sleep. Centers for Disease Control and Prevention. https://www.cdc.gov/media/releases/2016/p0215-enough-sleep.html. Published February 16, 2016. Accessed March 1, 2021.
- Common Sleep Disorders: Symptoms, Causes & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/11429-common-sleep-disorder. Accessed March 1, 2021.
- Gottlieb DJ, Redline S, Nieto FJ, et al. Association of Usual Sleep Duration With Hypertension: The Sleep Heart Health Study. Sleep. 2006;29(8):1009-1014. doi:10.1093/sleep/29.8.1009
- Torborg L. Mayo Clinic Q and A: Lack of sleep and risk of high blood pressure. Mayo Clinic. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-lack-of-sleep-and-risk-of-high-blood-pressure/. Published January 28, 2017. Accessed March 1, 2021.
- Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertension Research. 2012;35(7):695-701. doi:10.1038/hr.2012.26
- Calhoun DA, Harding SM. Sleep and hypertension. Chest. 2010;138(2):434-443. doi:10.1378/chest.09-2954
