Study Title: Efficacy Versus Effectiveness in the Treatment of Obstructive Sleep Apnea: CPAP and Oral Appliances
Authors: Kate Sutherland, Craig L. Phillips, Peter A. Cistulli
Background:
Obstructive sleep apnea (OSA) has become increasingly prevalent in recent years, in part due to the rise in obesity. The condition, which involves upper airway obstruction during sleep, causes disrupted sleep and hypoxia. As a result, people with OSA experience a higher risk of all-cause mortality, as well as
- Daytime sleepiness
- Reduced quality of life
- Workplace accidents
- Motor vehicle accidents
- Hypertension
- Cardiovascular disease
- Type 2 diabetes
People with OSA need effective, long-term treatment options, both to alleviate OSA symptoms and to prevent the serious health risks linked to this dangerous sleep disorder. When treating patients with chronic conditions like OSA, health care providers select treatments that offer the best long-term health outcomes. Providers need to distinguish between treatment efficacy and treatment effectiveness, which are how well treatments work under ideal and real-world conditions, respectively.
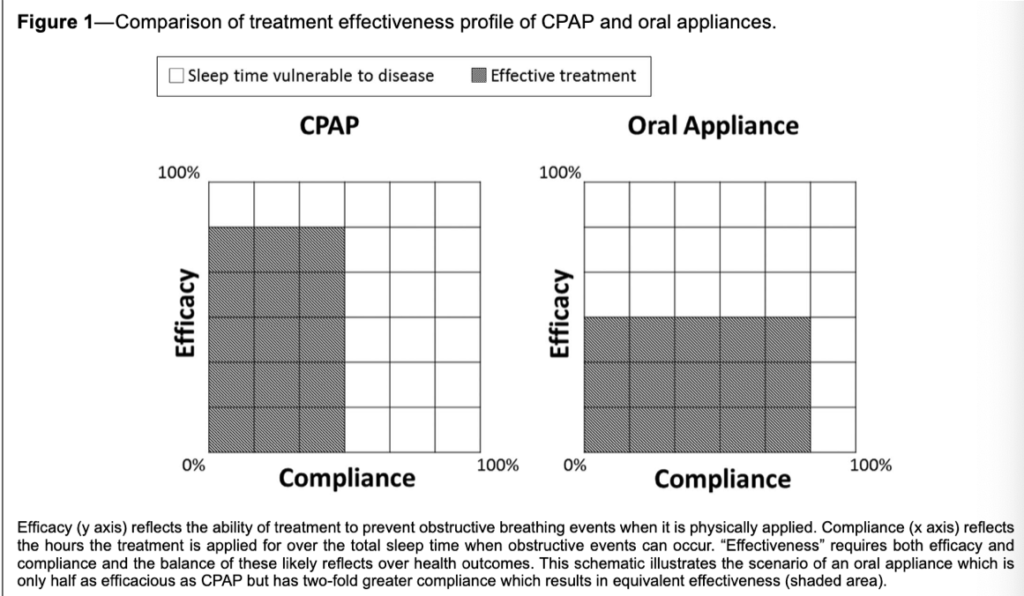
Continuous positive airway pressure (CPAP) therapy, which uses pressurized air to open collapsed airways, is the standard OSA treatment because of its high efficacy. However, low compliance from patients often undermines CPAP therapy’s long-term effectiveness. Oral appliance (OA) therapy, which dentists can custom fit for patients, offers an alternative treatment for OSA.
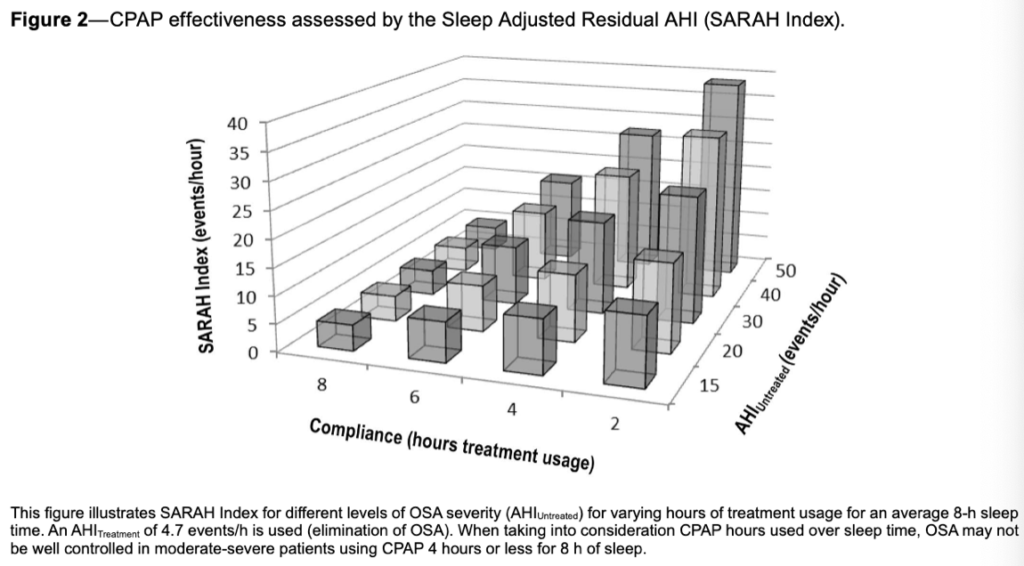
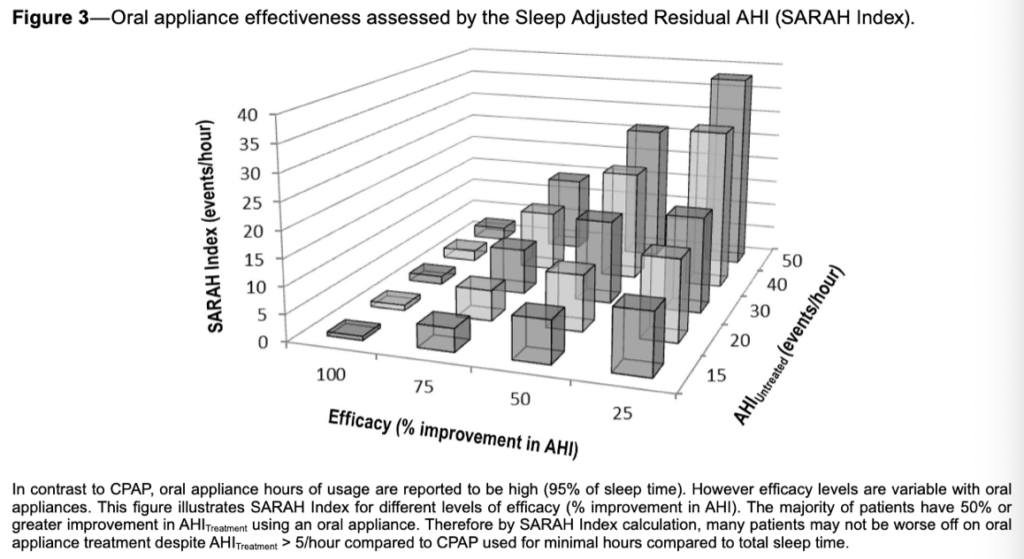
When studying the effectiveness of these 2 treatments, patient compliance can be represented as a ratio of treatment usage to total sleep time. Understanding the impact usage rates have on each treatment’s overall effectiveness helps illustrate their potential outcomes in real-world settings.
Study Objective:
To compare the overall treatment efficacy and effectiveness profiles of CPAP therapy and OA therapy using measures of patients’ apnea-hypopnea index (AHI) versus their Sleep Adjusted Residual AHI (SARAH Index). The objective measurement of OSA treatment effectiveness represents the combined effect of treatment efficacy and patient compliance for patients with OSA.
Methodology:
This study used objective data downloads from CPAP machines and objective compliance monitors for oral appliances to verify patient usage patterns. The analysis incorporated data from 108 participants with moderate-severe OSA who received 1 month of each optimized treatment: CPAP and OA therapy. Treatment efficacy and effectiveness were calculated and compared using the AHI and the SARAH Index.
Results:
- Between CPAP and OA therapy, patients with moderate-severe OSA experienced no significant differences in health outcomes, including measures of cardiovascular health, neurobehavioral indicators, or quality of life
- Hypertensive patients experienced reduced blood pressure during sleep when using each treatment
- While OA therapy had lower efficacy, CPAP therapy had significantly lower usage rates
Treatment with OA therapy resulted in residual OSA compared with CPAP therapy (AHI 4.5 ± 6.6 vs 11.1 ± 12.1/h); however, on average, OA therapy users reported an additional 1.3 hours of usage (95% of sleep time) and 50% improvement in AHI.
Conclusion/Discussion:
The results of this study indicate how OA therapy, despite its lower efficacy, can deliver similar real-world health outcomes as CPAP therapy. In controlled settings, CPAP therapy consistently reduces patients’ AHI. However, the higher usage rates of OA therapy (+1.3 hours per night) increased the overall effectiveness, especially for patients with poor CPAP compliance or longer sleep periods. Median treatment AHI for CPAP therapy was 4.7 hours; however, up to 50% of OSA patients use CPAP therapy for less than 4 hours per night. Additionally, as patients saw similar improvements in daytime sleepiness, nighttime hypertension, and overall quality of life, OA therapy’s real-world effectiveness may outweigh CPAP therapy’s clinical efficacy for patient health.
References:
- Sutherland K, Phillips CL, Cistulli PA. Efficacy versus effectiveness in the treatment of obstructive sleep apnea: CPAP and oral appliances. J Dent Sleep Med.2015;2(4):175-181. doi.org/10.15331/jdsm.5120
