This is the time of year for new year’s resolutions. People take this time to improve their health by joining a gym, cutting out processed foods, or just plainly visiting their physician more often. One new year’s resolution that could lead to better sleep and better health for your cardiac patients is sleep apnea evaluation. This sleep disorder is common among patients with cardiovascular disease and contributes to increased morbidity and mortality. Cardiac patients often suffer from sleep apnea, but unfortunately too commonly it remains undiagnosed.
Pathophysiology of Sleep Apnea
There are two types of sleep apnea:
- Obstructive sleep apnea: airflow obstruction due to nocturnal relaxation of pharyngeal muscles.
- Central sleep apnea: nocturnal neurologic cessation of all breathing effort.
Obstructive sleep apnea
Obstructive sleep apnea (OSA), caused by physiologic aspects of patients, is more common among obese and patients with coronary disease. Despite the disorder’s prevalence, it is often missed during exams, and often goes undiagnosed.
OSA episodes have many detrimental consequences, including lower oxygen levels, due to obstructed airways. Obstructed airways also cause exerted abdominal effort, which causes changes in intrathoracic pressure and leads to oxidative stress. OSA also leads to constriction as well as increased pressure of pulmonary veins.
This causes the cardiac load to increase, which is very damaging to patients with a coronary disease whose hearts are already working overtime dramatically. OSA episodes cause a swing in intrathoracic pressure, which results in a decrease in cardiac output and is worse during REM sleep. Decreased cardiac output can ultimately lead to cardiogenic shock.
Central sleep apnea
Central sleep apnea (CSA) as opposed to obstructive sleep apnea, does not include thoracoabdominal effort. While physiologic in some cases, CSA is more often caused by sensitive chemo responses due to alterations in carbon dioxide levels. These alterations can be a result of arousal from sleep. In CSA episodes, Hunter-Cheyne-Stokes respiration can occur, which is a cyclical crescendo-decrescendo respiratory effort. This type of respiration is worse during NREM sleep.
Sleep apnea is more prevalent than one might think, affecting 30-60% of patients with underlying coronary disease and cardiovascular risk conditions such as diabetes, hypertension, and heart failure. Patients with underlying conditions such as coronary disease are more likely to
develop sleep apnea, but may not be aware of it, which is why it is crucial to suggest that patients get tested.
Sleep Apnea and Cardiac Health
Both forms of sleep apnea are common in patients with underlying cardiovascular conditions.
Patients with heart failure have been shown to have fluid in the neck and alveoli of the lungs. This shift of fluid causes pharyngeal edema, nearly causing OSA. Episodes of OSA impair diastolic function and cause atrial and aortic enlargement. REM-related OSA, in particular, is associated with an increased risk for cardiovascular complications.
Patients with heart failure may also develop pulmonary congestion, which could cause CSA. Sleep apnea causes overworking of the heart and could potentially cause cardiovascular problems, if not worsen those already present. Sleep apnea tests should be suggested to patients with underlying conditions to reduce the risk of further heart damage.
Effects of Sleep Apnea
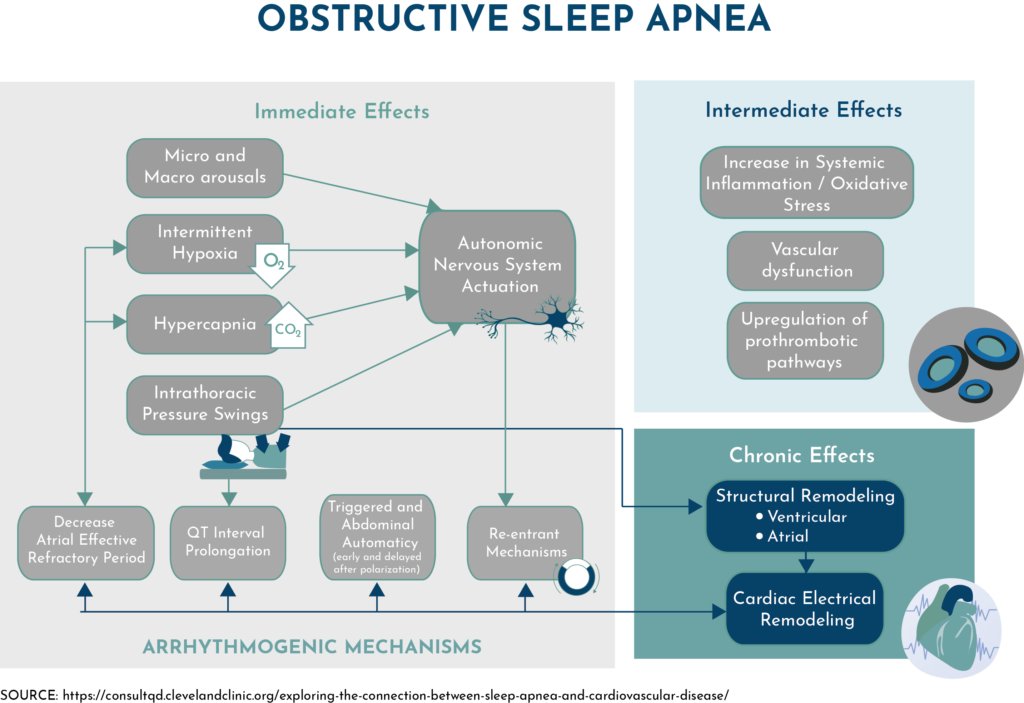
Sleep apnea effects include, but are not limited to, lower oxygen levels, increased cardiac output, and increased blood pressure. All of these symptoms are harmful, especially to patients with coronary disease. The effects of obstructive sleep apnea in cardiac patients can be ranked as immediate, intermediate, and chronic. Direct effects include lower oxygen and carbon dioxide levels, intrathoracic pressure swings, and fluctuations in the autonomic nervous system.
Intermediate effects include systemic inflammation, oxidative stress, vascular dysfunction, and upregulation of prothrombotic pathways. Chronic effects of sleep apnea include cardiac electrical and structural remodeling. Patients with sleep apnea typically have fatigue, headaches, memory impairment, and tend to snore at night.
A simple questionnaire for cardiac patients can determine if sleep apnea tests are needed and can serve as a future reference if these symptoms develop later on. Educating patients on the causes, symptoms, and effects of sleep apnea can help decrease this disorder’s prevalence.
Getting Tested
Although sleep apnea is associated with many cardiovascular complications, it can often go undiagnosed.
That’s where WatchPAT® ONE can help. Patients can use this test in the comfort of their own beds (especially important in light of the COVID-19 pandemic) and in just a few simple steps, complete their sleep study. Once the test is complete, physicians can review the automatic results and discuss them with the patient.
With no wait time for the test or the results, no risk of exposure, and no need to mail in any part of the device, WatchPAT® ONE provides a simple solution for your cardiac patients.
As cardiac patients are vulnerable to sleep apnea, among other conditions, take the opportunity to recommend sleep apnea tests. Diagnosing sleep apnea is the first step to keeping a patient’s health under control and reducing the risk of further complications. A proper diagnosis and taking the time to educate patients is what will get them on the right path toward appropriate treatment and better health.
